Bill With Bipartisan Support Would Eliminate Out-Of-Pocket Costs For Advanced Breast Cancer Screenings
ST. Paul, Minn. (WCCO) -- A proposal in the Minnesota Legislature would eliminate out-of-pocket costs for advanced testing that could detect early signs of breast cancer in a move supporters say will break down barriers keeping women from preventive care.
The single-page bill says broadly that if a provider determines a patient needs additional diagnostic services or testing following a mammogram, a health plan must provide those screens with no cost sharing, including co-pay, deductible or coinsurance. That includes Medical Assistance and MinnesotaCare, programs providing coverage for low-income people in the state that were added in the bill during the legislative process.
Breast cancer is the second most common cancer found in women, behind skin cancers.
An estimated 16% of people who receive annual screening mammograms get called back for diagnostic imaging, which is more expensive, according to the Susan G. Komen Breast Cancer Foundation that studied the issue. Patients can pay anywhere from hundreds to more than $1,000—even with insurance—for more advanced tests, the organization said.
Rep. Patty Acomb, DFL-Minnetonka, wrote the bill because of her own personal battle with the disease, which she says is the reason she ran for office. Five years later, she's triumphed, following six months chemo, 40 rounds of radiation and a lumpectomy.
"I needed follow up testing in order to get conclusive results and those follow up tests came with co-pays," recalled Acomb. "While I could pay them, it seemed like there would certainly be people who might not be able to pay them."
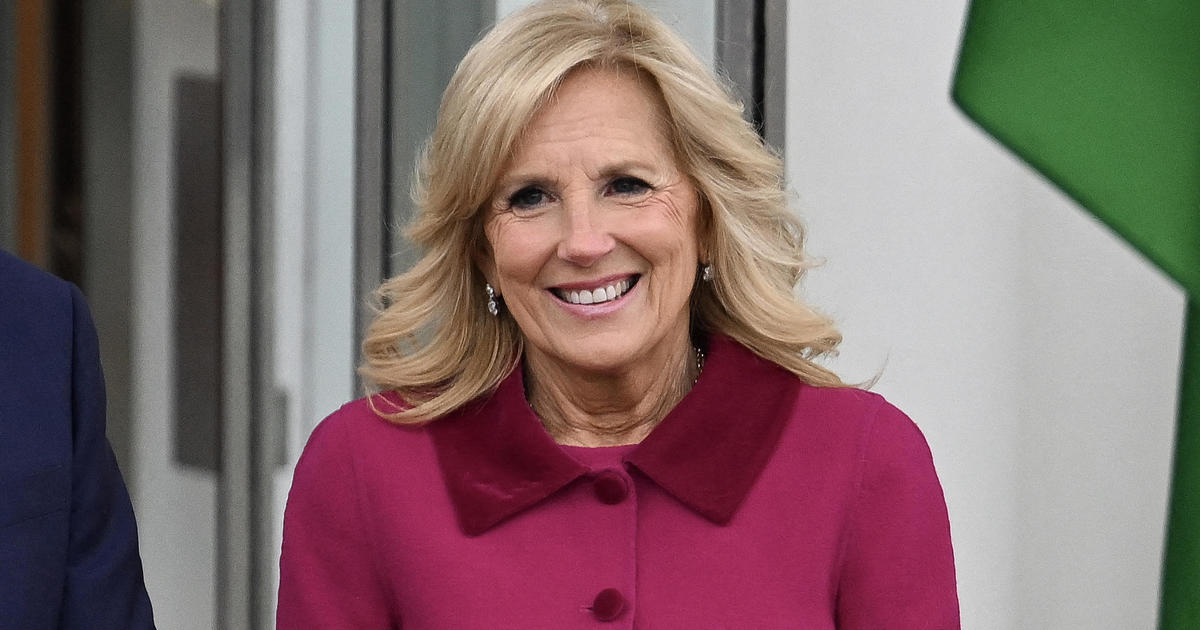
Acomb reached out to Sen. Carla Nelson, R-Rochester, for her support in the Senate. Nelson said working on the bill prompted her to get checked and an advanced diagnostic test—which she fought her insurance company to cover—detected the earliest stages of breast cancer.
Both say their personal stories underscore that early detection is critical and they hope they can empower women to seek testing that could save their lives.
"I'm so thankful, so blessed, that I was able to get such early diagnosis and treatment," said Nelson." It makes a world of difference. As leaders we want to make sure every woman has that chance."
Nelson pointed to an analysis from the Minnesota Department of Commerce that determined the bill would not create a new state mandated benefit, but rather clarifies "existing benefits under health plans by requiring them to be covered at a zero-cost preventive level."
"By eliminating that barrier, patients may be able to obtain additional services and receive earlier diagnoses for cancer," the report said.
Shaunequa James, program manager at Gilda's Club Twin Cities, a nonprofit that offers emotional and social support to cancer patients, said she thinks passing the legislation is a step towards health equity.
Too often she sees people priced out of preventive care, especially men and women of color.
"This could be a turning point for people seeking the care that they need and actually getting it," she said. "So cost isn't a factor that keeps them away from it."
The proposal is moving through committees in the Minnesota House but hasn't gotten a hearing in the Minnesota Senate, though Nelson hopes it will.
"It's not a political issue," she said. "It's a human dignity issue."